Oral glucose-lowering agents in type 2 diabetes mellitus (T2DM)


Oral glucose-lowering agents in type 2 diabetes mellitus (T2DM)
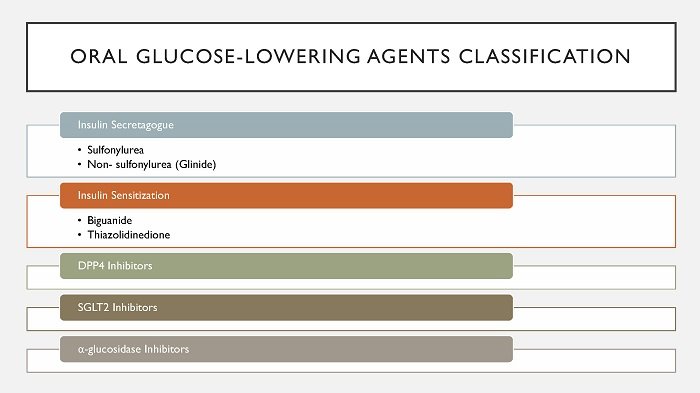
Oral glucose-lowering agent in Thailand categorized into 5 groups according to different mechanism of action as follows:
1. Insulin secretagogue (increase secretion of insulin)
a. Sulfonyl urea e.g. Glipizide, Glibenclamide, Glicazide, Glimepiride
b. Non-sulfonylurea or Glinide e.g. Repaglinide
2. Insulin sensitization (decrease insulin resistance)
a. Biguanide e.g. Metformin
b. Thiazolidinedione e.g. Pioglitazone
3. DPP4 inhibitors (increasing postprandial active incretin by inhibit DPP4 activity) e.g. Sitagliptin, Vildagliptin, Saxagliptin, Linagliptin, and Alogliptin
4. SGLT2 inhibitors (block glucose reabsorption by the kidney) e.g. Dapaglifozin, Empaglifozin
5. Alpha-glucosidase inhibitors (slow intestinal carbohydrate digestion/absorption) e.g. Acobose, Voglibose
Nowadays the long-term management of DM recommends setting HbA1c level target individually. Normally, the HbA1c target is < 7%. However, the physicians might consider less stringent HbA1c goal target (7-8%) for elderly patients, patients with long-standing diabetes, advanced microvascular/macrovascular complications, extensive comorbid conditions, history of severe hypoglycemia, or limited life expectancy3,4. In addition, more stringent HbA1c target level (<6.5%) is also appropriate for selected individual patients if this can be achieved without significant hypoglycemia or other adverse effects of treatment. The appropriated patients might include those short durations of DM, long-life expectancy, or no significant cardiovascular disease3,4. Moreover, the study founds controlling HbA1c target level <7% in patient with short duration of DM, no complication, or extensive comorbid conditions, can reduce short-term and long-term microvascular complications, also with long-term macrovascular complication5-7.
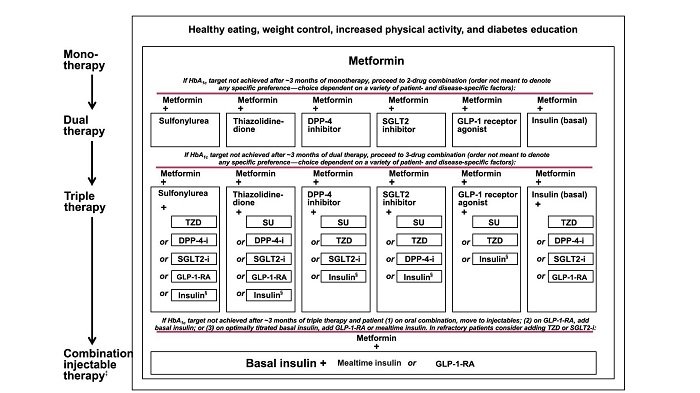
Metformin is the first line drug for most patients2,4 (contraindication if GFR<30 ml/min/1.73m2)8. It reduces hepatic glucose production, less hypoglycemia possibilities, and no weight gain. However, long-term treatment with Metformin can reduce intestinal absorption of vitamin B122,9.
How to use oral glucose-lowering agent in type 2 diabetes mellitus (T2DM)
The physician should use oral glucose-lowering agents together with lifestyle modification. To start treatment with oral glucose-lowering agents depends on level of fasting plasma glucose (FPG), HbA1c level, hyperglycemic symptoms, diabetes complications, patients health status (obese, liver disease, renal function), and pregnancy plan (in woman).
1. In case of high blood glucose level, the physician should evaluate for any emergency stage such as Diabetes Ketoacidosis (DKA) or Hyperglycemic Hyperosmolar State (HHS) by additional blood test. If there is no emergency stage but patients have hyperglycemic symptoms, the combination of insulin should be taken in to consideration1,2. In some cases that need to reduce blood glucose level with limited time such as patients who have infection or the patient who is going to have operation, they need to treat with high efficacy anti-diabetic agents for improve glucose level within limited time.
2. If the first diagnosis shows that HBA1c ≥9%, the physician can start treatment with combination oral glucose lowering agents (different mechanism)1.
3. If the patient cannot achieve goal by metformin monotherapy, the physician can add the 2nd anti-diabetic agent, by consider
a. Efficacy: The efficacy of oral glucose-lowering agents is different; for example, sulfonylurea and thiazolidinedione have high efficacy, while DPP-4 inhibitor and SGLT2 inhibitor have intermediate efficacy on glycemic control1.
b. Side effect:
i. Hypoglycemia: hypoglycemia often occurs in patients who take sulfonylurea, especially Glibenclamide. While, the new generation of sulfonylurea found less hypoglycemia e.g. Glimepiride10.
ii. Weight gain: thiazolidinedione and sulfonylurea can induce weight gain but DPP4 inhibitors provide weight neutral. While, weight loss could be seen in the patients who take SGLT2 inhibitors1.
iii. Others adverse events:
- thiazolidinedione: edema/heart failure, bone fracture1,2.
- SGLT2 inhibitors: urinary tract infection, vulvovaginitis, euglycemic DKA1,2.
- alpha-glucosidase inhibitors: GI side-effect1,2.
- SGLT2 inhibitors: urinary tract infection, vulvovaginitis, euglycemic DKA1,2.
- alpha-glucosidase inhibitors: GI side-effect1,2.
c. Price:
There is an ongoing study “Glycemic Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE)”11 aims to evaluate effectiveness of second add-on to Metformin. The study compares 4 major drug classes, which are sulfonylurea, DPP4 inhibitors, GLP-1 Receptor Agonist and Basal insulin. The study will compare over 4 years on glycemic control and other medical, psychosocial, and health economic outcomes11.
Moreover, stage of diabetes should be taken in to consideration as well e.g. insulin secretagogue agent is not suitable for the patient with long standing diabetes. Furthermore, the physicians need to evaluate that high HbA1c is affected by ‘fasting hyperglycemia’ or ‘post-prandial hyperglycemia’ in order to choose the suitable oral glucose-lowering agent for the patients.
There is an ongoing study “Glycemic Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE)”11 aims to evaluate effectiveness of second add-on to Metformin. The study compares 4 major drug classes, which are sulfonylurea, DPP4 inhibitors, GLP-1 Receptor Agonist and Basal insulin. The study will compare over 4 years on glycemic control and other medical, psychosocial, and health economic outcomes11.
Moreover, stage of diabetes should be taken in to consideration as well e.g. insulin secretagogue agent is not suitable for the patient with long standing diabetes. Furthermore, the physicians need to evaluate that high HbA1c is affected by ‘fasting hyperglycemia’ or ‘post-prandial hyperglycemia’ in order to choose the suitable oral glucose-lowering agent for the patients.
Dr. Wanas Chaitree
Reference
1.American Diabetes A. 7. Approaches to Glycemic Treatment. Diabetes Care 2016;39 Suppl 1:S52-9.
2.Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm - 2016 Executive Summary. Endocr Pract 2016;22:84-113.
3.American Diabetes A. 5. Glycemic Targets. Diabetes Care 2016;39 Suppl 1:S39-46.
4.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140-9.
5.Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:854-65.
6.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837-53.
7.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359:1577-89.
8.http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm494829.htm.
9.de Jager J, Kooy A, Lehert P, et al. Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. BMJ 2010;340:c2181.
10.Korytkowski MT. Sulfonylurea treatment of type 2 diabetes mellitus: focus on glimepiride. Pharmacotherapy 2004;24:606-20.
11.Nathan DM, Buse JB, Kahn SE, et al. Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care 2013;36:2254-61.
